

It is important the ambulance clinician carefully assesses the patient and environment to reach a reasoned conclusion to why the fall has taken place and then take steps to reduce the likelihood of it happening again, which may involve routine, urgent or emergency referral to another professional. Health problems that increase the risk of falling There are a range of potential causes of falls in adults including 1 :Ī history of falls and associated problems such as fear of falling and associated injuries After discharge Ian will return to his GP for long-term re-adjustment to his anti-hypertensive medication. You decide to convey Ian to hospital where it is later confirmed his bradycardia and hypotension was a side effect of bisoprolol, so the next dose was withheld and he remained systemically well. Ian is stable for the rest of contact with the ambulance crew. Supine blood pressure is 110/75 and Ian has no dizziness so able to slowly stand up and sit on a chair. You reassess Ian his heartrate is now 87, regular and the 12 lead ECG shows a sinus rhythm with no other abnormalities. Maureen monitors Ian’s ECG and you see an almost instant increase in his heartrate and a reduction in pallor. Transcutaneous pacing may also be required.Īn intravenous cannula is easily placed and a 600mcg atropine bolus is given. Emergency treatment includes identification and management of the underlying cause, ensuring adequate oxygenation and medications such as atropine. She explains that in an adult, a heart rate under 60 is called bradycardia and can have causes including heart disease and toxicity from prescribed medications.

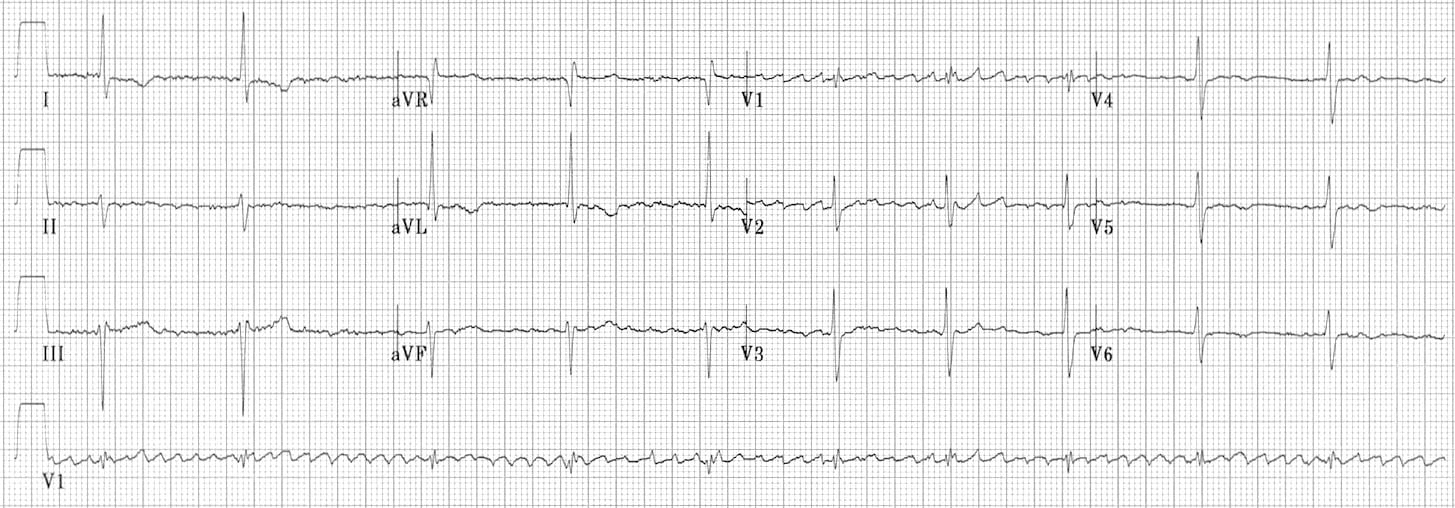
Maureen reviews the situation to form a diagnosis of symptomatic bradycardia, which could be related to recent medication changes. He also takes amlodopine, simvastatin and aspirin but not allergic to any medication. In addition to high blood pressure, Ian has hyperlipidaemia. Since then, Ian says he has felt dizzy on exertion but was not very worried about it until today. Maureen learns that Ian recently saw his GP regarding poorly controlled hypertension and the reading was 182/111, so his bisoprolol was increased from 5mg to 10mg daily. Not give oxygen: Ian’s saturations maintain at 97% on air, in line with British Thoracic Society guidelines and you and Maureen can concentrate on evidence based interventions to manage his condition. Maureen quietly comments how studies have shown patients do not benefit, and may even do worse, when oxygen is given unnecessarily. You find it harder to hear Ian over the whooshing noise while hoping not to need a lot of oxygen for hypoxic patients later on in the shift. His saturations rapidly climb to 100% but he does not feel better and other observations do not improve. Give oxygen: You place Ian on 15lpm oxygen through a non-rebreathing mask. What are you going to do: Give Ian oxygen or not give oxygen? No apparent intoxication with alcohol or illicit drugs Pupils equal and reactive, 5mm bilaterally Occasional ventricular escape beats with wide QRS complexes but no other changes Ian is still laid, almost supine, beside his seat at the dinner table propped up by a few pillows.ġ2-lead ECG: sinus bradycardia with 1 st degree heart block. You and Maureen enter the dining room the only danger is the delicious looking roast dinner displayed on the table it would be easy to become distracted and tuck in! The last time Ian fell they were very concerned so told him to stay on the floor until an ambulance arrived. They say he has looked pale all day and has fallen several times before struggling to stand again.

On arrival, you’re met by the patient’s family who explain `Ian` is visiting for Sunday lunch. You’re simply wondering if patient report forms should a copy and paste function. Whilst calls for fallen patients are common (you’ve already done three that shift), Maureen comments this patient is a little younger than the normal tumbled client and may have an underlying reason they have fallen repeatedly. Follow him on Twitter through the Sunday shift, the mobile data terminal alerts you and Paramedic Maureen to a `64 year old male Patient keeps falling and can’t get up`. This blog post was written by Matt Green, a paramedic for an NHS Trust.


 0 kommentar(er)
0 kommentar(er)
